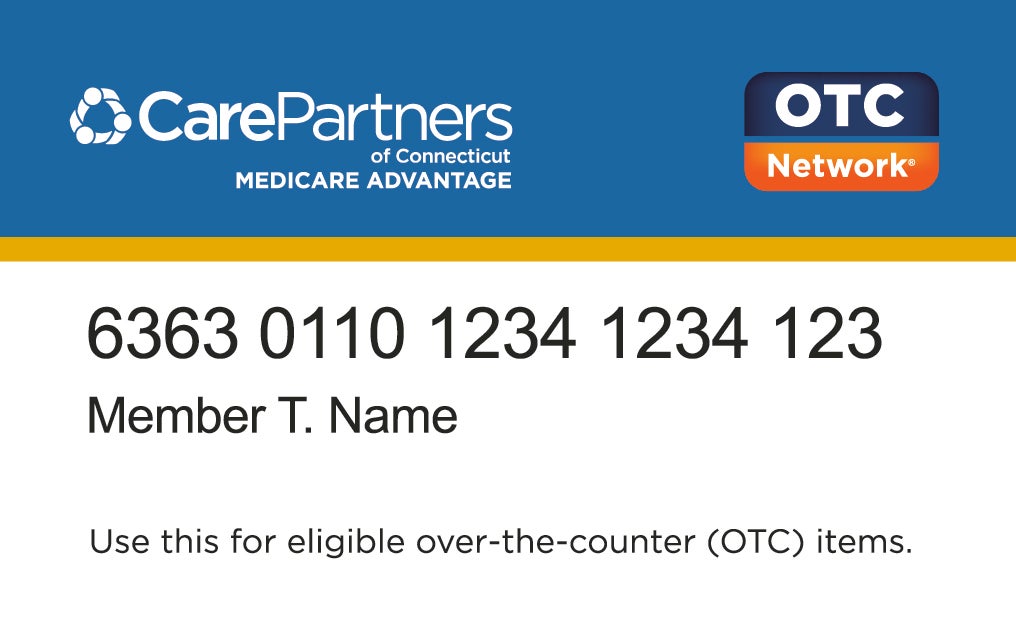
How Your CarePartners of Connecticut Over-the-Counter (OTC) Benefit Works

CarePartners of Connecticut plan members have access to savings on eligible over-the-counter (OTC) medicines and health-related items by using your OTC benefit.
How Your OTC Benefit Works
At the beginning of each calendar quarter, your OTC card is loaded with the quarterly OTC amount for your plan.1
Your balance does not carry over—Try to spend the full amount before the end of each quarter.
Don’t throw out your card—It will be reloaded at the start of the next calendar quarter.
Disclaimer: Eligibility of items may change due to regulatory or other changes. Prices may vary from store to store.
| Plan | 2025 Amount | 2026 Amount | Quarter |
| CareAdvantage Preferred (HMO) | $140 $140 $140 $140 | $50 $50 $50 $50 | Jan-Mar Apr-Jun Jul-Sep Oct-Dec |
| *CarePartners Access (PPO) | $102 $102 $102 $102 | $50 $50 $50 $50 | Jan-Mar Apr-Jun Jul-Sep Oct-Dec |
| *Access PPO members receive a Visa® Flex Advantage spending card to access your OTC benefit. For information about using this card, visit carepartnersct.com/FlexAdvantage. | |||
Click Here to view the 2026 OTC Benefits Medline Catalog
Click Here to view the 2026 OTC Item Catalog
For More Information
If you have any technical difficulty using your card, call Medline at 1-833-569-2331.
If you have any questions about using your OTC benefit, call CarePartners of Connecticut Member Services at 1-888-341-1507(HMO)/1-866-632-0060 (PPO)(TTY: 711).
1Quarterly OTC credit is for the purchase of Medicare-approved OTC items from participating retailers and plan-approved online stores. Unused balance at the end of a calendar quarter does not roll over. Under certain circumstances, items may be covered under your Medicare Part B or Part D benefit.


